Be advised that we have closed our Holland’s Drug location on South Locust Avenue.
Please contact one of our other two locations for assistance with your prescription information.
We look forward to continuing to serve you. Thank you!
Get Healthy!
- Posted September 19, 2025
Neuromuscular Disease Care Is Entering a New Era of Hope and Innovation
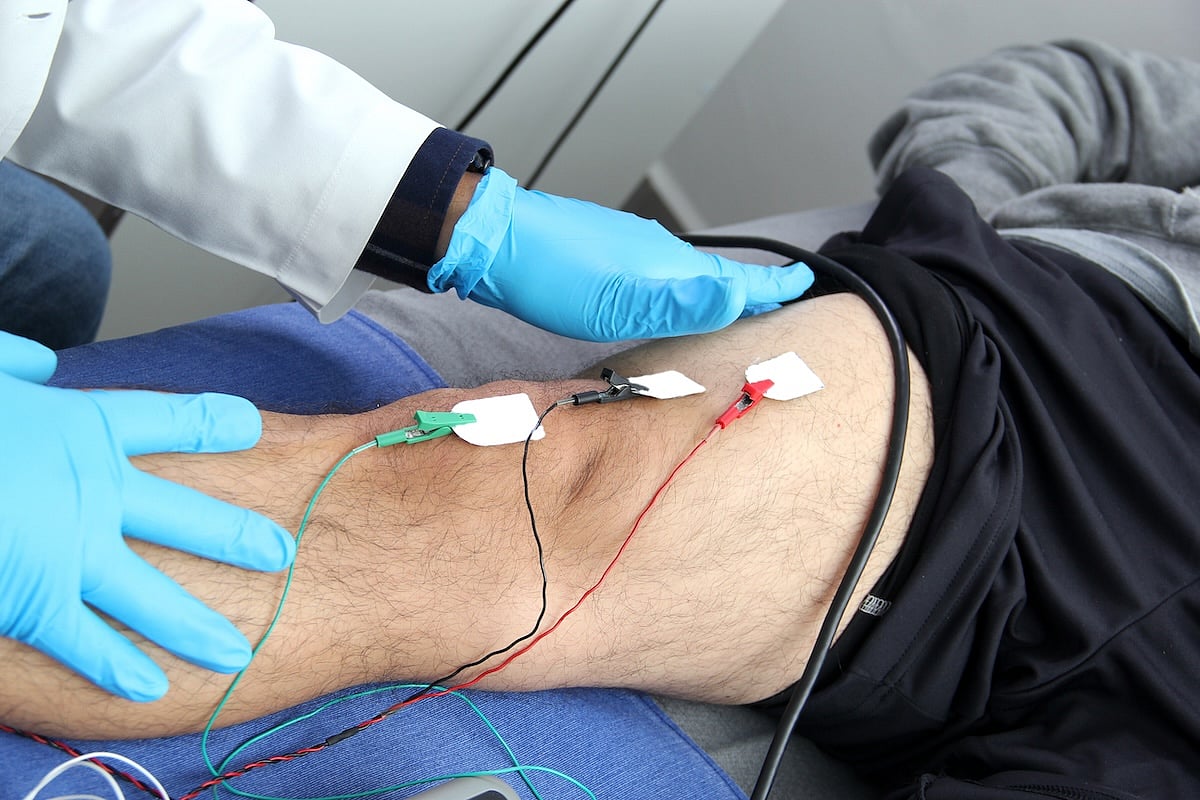
Every movement we make, whether walking, speaking or even breathing, depends on the health of our muscles and nerves.
For people living with one of the more than 300 rare conditions known as neuromuscular diseases (NMDs), those everyday actions can become extraordinary challenges.
While these diseases such as muscular dystrophies, amyotrophic lateral sclerosis (ALS), Charcot-Marie-Tooth disease (CMT), myotonic dystrophy, oculopharyngeal muscular dystrophy (OPMD), ataxias and limb-girdle muscular dystrophy (LGMD) can cause muscle weakness, loss of mobility and breathing problems, the pace of research is bringing new hope.
For most of human history, people living with neuromuscular diseases have had few, if any, treatment options.
Today, dozens of treatments are already available, with many more in the pipeline that alter the course of their disease progression.
What are neuromuscular diseases?
Neuromuscular diseases happen when there’s a problem with the muscles themselves or the nerves that control them. These issues can be caused by genetic changes, immune system attacks or other, unknown factors.
Some conditions, like Duchenne muscular dystrophy, often begin in early childhood. Others, like ALS, usually appear in adulthood. Still others, such as CMT or myotonic dystrophy, may progress slowly over decades.
These diseases can look very different from one another, but they share a common challenge: They make it harder for the body to move, speak, swallow and, in severe cases, breathe.
The power of early diagnosis
Finding these diseases early can make a big difference. Some states have added Duchenne muscular dystrophy to their newborn screening panels, with efforts underway to include it nationwide.
When a disease is found before symptoms appear, treatments and interventions can start earlier, often leading to better long-term outcomes.
This is already true for neuromuscular conditions like spinal muscular atrophy (SMA) and Pompe disease, both of which are on the Recommended Uniform Screening Panel (RUSP) and are included in newborn screening across all 50 states.
Breakthroughs across the neuromuscular field
Right now, neuromuscular research is entering one of the most promising eras we have ever had. Dozens of new therapies are already changing lives, and many more are on the horizon, offering the possibility not just of slowing disease but of restoring strength.
In recent years, the U.S. Food and Drug Administration (FDA) has approved a wave of new therapies, including gene therapies, RNA-targeted drugs, and small molecules that support muscle and nerve function in the context of disease. Many more are in late-stage trials.
Some examples include:
Duchenne muscular dystrophy (DMD) — New gene therapies designed to replace or repair faulty dystrophin genes are showing encouraging results.
Charcot-Marie-Tooth disease (CMT) — Experimental drugs are targeting the root genetic causes, with the potential to protect nerve function.
Myotonic dystrophy (DM) and oculopharyngeal muscular dystrophy (OPMD) — Researchers are developing RNA-based treatments to correct the harmful effects of repeat expansions in DNA.
Ataxias (such as Friedreich’s ataxia or FA) — Therapies in testing aim to improve balance, coordination and nerve signaling.
Limb-girdle muscular dystrophy (LGMD) — Multiple gene therapy candidates are being designed for specific LGMD subtypes.
This is one of the most exciting times in neuromuscular research. Progress is being made not just in slowing disease, but in potentially restoring strength and function.
The next frontier: Muscle regeneration and biomarkers
Scientists are now exploring ways to help the body repair or rebuild muscle that has already been lost. Some therapies, like myostatin, block proteins, which limits muscle growth, to encourage muscle building. Others use stem cells or regenerative medicine to try to replace damaged muscle fibers.
At the same time, new biomarkers, measurable signs of disease progression or treatment response, are being identified. These can help doctors track how well a therapy is working so they are able to adjust treatment plans sooner.
Biomarkers are game-changers, because they provide a clearer picture of what’s happening in the body, often before symptoms change.
Better access to care
During an observance during September called Telehealth Awareness Week, experts highlight how virtual care can connect patients with top specialists, no matter where they live.
This is especially important for people with rare neuromuscular diseases, who may need to travel long distances to reach expert clinics.
The MDA Care Center Network is in more than 150 top medical institutions nationwide and many offer both in-person and telehealth visits, helping more families get timely access to multidisciplinary care.
MDA’s role in powering progress
For 75 years, the Muscular Dystrophy Association’s (MDA) research program has led to many of today’s treatments and is now fueling the next wave of innovation.
The organization has invested more than $1 billion in research, supports more than 150 MDA Care Centers, and works with policymakers to expand newborn screening and treatment access.
In September, multiple awareness days and observances draw attention to these diseases, offering an important moment to highlight the progress being made.
The month includes Muscular Dystrophy Awareness Month, Newborn Screening Awareness Month, and disease-specific events such as World Duchenne Day (Sept. 7), Myotonic Dystrophy Awareness Day (Sept. 15), Telehealth Awareness Week (Sept. 15–21), OPMD Awareness Day (Sept. 23), International Ataxia Awareness Day (Sept. 25), and LGMD Day (Sept. 30).
Through the MDA Strong Campaign, the Muscular Dystrophy Association is not just raising awareness; we’re showing how decades of scientific progress are transforming lives and empowering families to live longer, more independent lives.
About the expert
Brian Lin, PhD, is a Research Portfolio Director at the Muscular Dystrophy Association (MDA), where he oversees research focused on neurology-based diseases within the organization’s portfolio. He earned his PhD from the University of Maryland, Baltimore, studying UBQLN2 mutations in Amyotrophic Lateral Sclerosis (ALS) and Frontotemporal Dementia (FTD). Dr. Lin completed his postdoctoral training at the U.S. Food and Drug Administration (FDA), where his research focused on gene engineering and the role of synonymous mutations in protein therapeutics and gene therapies. His experience bridging molecular research and regulatory science now informs his work at MDA, where he supports cutting-edge research aimed at accelerating treatments and improving outcomes for individuals living with neuromuscular diseases.
